Clinical relevance
1. Endovascular aneurysm repair (EVAR) of infrarenal abdominal aortic aneurysms (AAA) is very common nowadays because EVAR compared to open surgery :
– Long-term outcomes ( rupture and survival rates ) is comparable
– Post-operative morbidity and mortality are lower
2. Concept of endoleak :
– Traditional open surgical repair : Tight sutures and hemostais are primarily achieved under direct visualization :
a) Swening of surgical graft at the proximal and distal ends of the aneurysm
b) Ligation or reanastomosis of arterial side branches originating from the aneurysmal sac ( e.g. IMA, lumbar arteries and accessory renal arteries )
– Endovascular aneurysmal repair : perigraft blood flow outside the endoprosthesis but inside the aneurysm sac may occur
Definition
1. Persistence of blood flow outside the lumen of the endoluminal graft but within an aneurysm sac
2. Due to incomplete exclusion of the aneurysm sac or vessel segment
3. As evidenced by imaging studies ( e.g. CT, USG, angiogram )
Classification of endoleaks
1. Endoleaks can be classified based on timing :
– Primary endoleaks ( < 30 days ) : Usually develop immediately after EVAR, and the aneurysm was never actually completely excluded from the arterial circulation
– Secondary endoleaks ( > 30 days ) : The aneurysm has been excluded from the arterial circulation primarily but endoleak was found upon follow-up imaging
2. Endoleaks can also be classified based on underlying cause :
– Type I : Attachment site leak
a) IA : Proximal
b) IB : Distal
c) IC : Iliac plug in aortouniiliac stent grafts
– Type II :
a) IIA : Reperfusion leak : Simple single inflow/outflow
b) IIB : Complex side branch perfusion
( Hyperdynamic on US = Quick wash-in; hypodynamic on US = Slow wash-in )
– Type III : Device-related leak
a) IIIA : Midgraft hole
b) IIIB : Junctional separation
c) IIIC : Any other leak caused by device failure
– Type IV : Porosity leak : Angiographic feature ( blushes ) rather than a true leak, occurs immediately after implantation for certain graft, but will resolve spontaneously within hours ( affected also by anticoagulation )
– Type V : Endotension
a) VA : Sac enlargement without demonstration of EL with any imaging modality
b) VB : Sac enlargement, currently no EL discernible, but type I or II EL in previous examinations
c) VC : Type I or III EL proven at surgery, not shown during follow-up imaging
d) VD : Type II EL proven at surgery, not shown during follow-up imaging

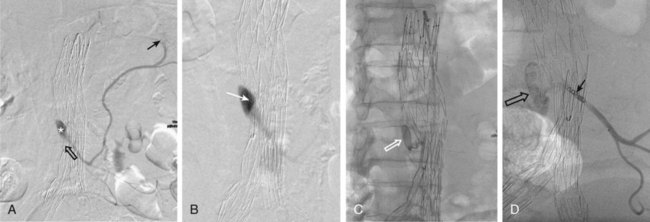
Examples :
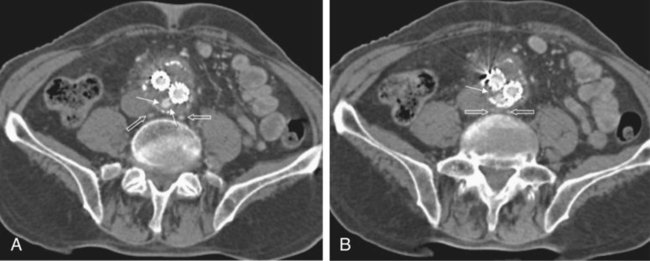
1. CT aortogram : Type IA endoleak ( small arrows ) with retroperitoneal hematoma ( open arrow )
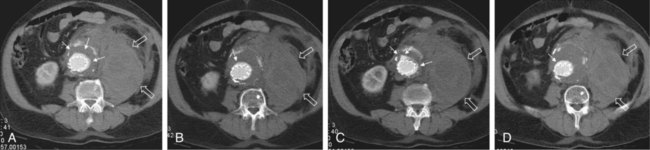
2. Angiography 18 months after EVAR : Type II endoleak ( star ) with feeding from from the right iliolumbar artery and outflow through the left iliolumbar artery ( arrows ). 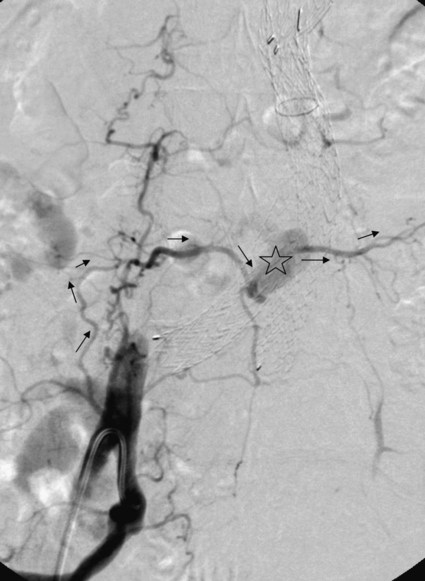
3. CT aortogram follow-up 12 months after endovascular repair : Dislocation of right iliac limb ( solid arrow in C ) from parent vessel ( open arrow ) causing type III endoleak ( arrows in A and B )
4. Angiography 18 months after endovascular repair : Right iliac limb has separated from stent-graft body ( arrows ) causing a type III endoleak ( open arrow ).

Significance of various types of endoleak
1. Type I endoleak : Usually due to improper patient selection such as :
a) Short aneurysmal neck
b) Severe angulation and calcification
c) Extensive thrombus lining of the neck
2. Type II endoleak : Development is a inherent phenomena of EVAR and is hardly be influenced by operation
3. Type III endoleak : More frequent with 1st and 2nd generation stent-grafts but decreased significantly with 3rd generation.
Diagnosis of endoleak
1. Post-EVAR patient follow-up imaging must indicate the following :
a) Morphologic evolution of aneurysmal sac : Maximal sac diameter
b) Any endoleak and its types
2. Possible imaging modalities for post-EVAR follow up :
CT, US, magnetic resonance imaging (MRI), intraarterial digital subtraction angiography (DSA), and plain abdominal radiology
Diagnosis of endoleak by CT
1. The most commonly used diagnostic imaging modality for post-EVAR patient follow-up
2. Multiphase examinations :
– Unenhanced : Differentiating small perigraft leaks from areas of calcified thrombus or metallic structures of the stent-graft
– Arterial phase : Detect most of the perigraft flow ( contrast extravasation )
– Delayed phase : Detect additional / clarify indeterminate perigraft flow ( contrast extravasation )
Example :
CT aortogram follow-up 6 months after EVAR.
A ( early arterial phase ) : Stent graft in-situ without endoleak
B ( delayed phase ) : Diffuse contrast enhancement in dorsal part of the aneurysmal sac ( arrows )
The aneurysmal sac in this case was not increased and thus these finding has no clinical consequence
3. Diagnostic features of endoleak in CT :
– Definition of endoleak = Contrast-enhancing area outside the stent-graft lumen but inside the aneurysmal sac
– Features to classify the types of endoleak :
a) Type I : Contrast-enhancing area is directly adjacent to the proximal and distal sealing zones
b) Type II : Presence of contrast-enhancing side branches which communicates with the contrast enhancement in the aneurysmal sac
c) Type III : Loss of stent-graft integrity, deformity, and migration which communicates with contrast enhancement in the aneurysmal sac
( Although metallic skeleton is typically evaulated in plain films )
Example :
CT artogram. Contrast enhancement within the aneurysmal sac ( arrow ) and enhanced lumbar arteries at the same level ( open arrows ), suggestive of a type II endoleak.
N.B. CT is unable to show the direction of flow as in angiography ( in this case is a inflow-outflow situation )
4. Drawbacks of CT :
– Radiation exposure : Serial CTs for long-term surveillance and requires multiphases
– Nephrotixic contrast medium needed in a considerable amount ( 80-120mL )
– Cannot display flow dynamics in feeding side branches
Diagnosis of endoleaks by USG
1. Most frequent alternative to multiphase CT in patient follow-up after EVAR :
– Less expensive
– No radiation or nephrotoxic contrast material is required (Fig. 50-7).
But its sensitivity and specificity are relatively lower than CT and cannot completely replace CT for surveillance
Example :
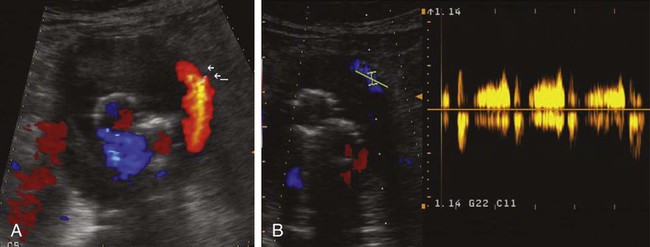
Color-doppler ultrasound.
– Transverse image : Large communicating type II endoleak (arrows) perfused via fourth lumbar arteries and inferior mesenteric artery.
– Spectral Doppler ultrasound : Pulsatile flow in the endoleak
Diagnosis of endoleaks by MRI
1. It does not expose the patient to radiation and nephrotoxic contrast media for long-term surveillance, besides, it has a higher sensitivity for contrast-induced signal changes reserved for challenging cases ( as less readily available then CT and USG )
Example :
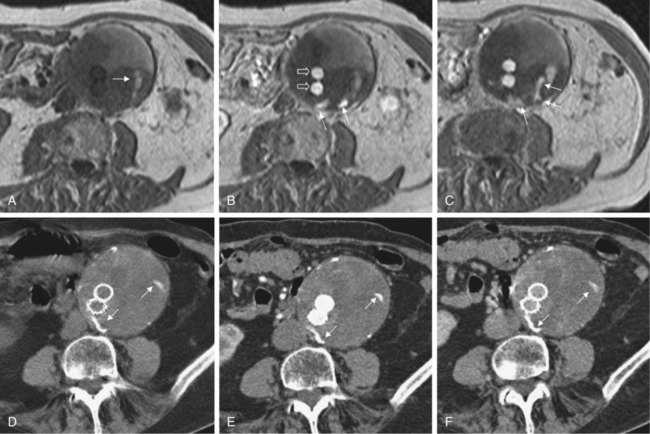
Dynamic contrast-enhanced MRI 12 months after endovascular repair :
– Non-enhanced phase (A) : Faint hyperintense area can be seen in left lateral part of aneurysm (arrow) that may be caused by fresh thrombus
– Arterial phase (B) : Both iliac limbs show intense enhancement with contrast material and are well perfused (open arrows), some contrast enhancement in aneurysmal sac ( white arrows )
– Delayed phase (C) : More obvious endoleak ( arrows )
Multiphase CT aortogram in the same patient on same day
– Unenhanced (D) : Aneurysmal sac is filled with inhomogeneous thrombotic material
– Arterial phase (E) and delayed phase (F) : Flakes of calcium (arrows) but no endoleak detected.
2. Drawbacks of MRI :
– Possible dislodgement and heating under high magnetic field
– Ferromagnetic component of compatible metallic implants cause susceptibility artifacts
Diagnosis of endoleaks by plain abdominal radiographs
1. Theorectically, endoleaks cannot be detected directly with plain abdominal films. However, change in the integrity ( e.g. progressive dilatation of components ), kinking or migration of stent-graft is an indicator of a possible endoleak.
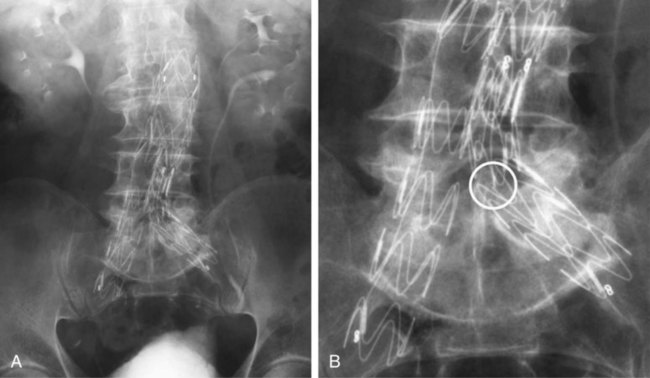
Example :
Plain abdominal film 24 months after EVAR. Obvious kink in left iliac limb, longitudinal connect bar is broken ( circle )
Diagnosis of endoleaks by intra-arterial angiography
This is not a routine procedure in patient follow-up after EVAR, but it has the following advantages for the following situations :
– Specific evaluation of each attachment site
– Demonstrate flow dynamics can be seen for proper endoleak classification
( e.g. Endoleak detected by CT in the vicinity of enhanced lumbar arteries can be type II, if flow in the lumbar artery is retrograde, or type I, if flow is antegrade )
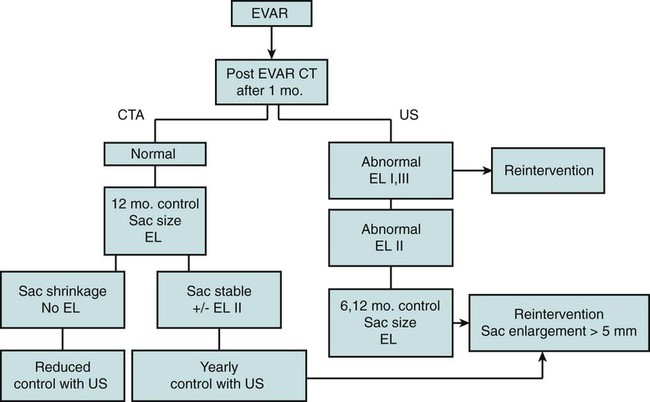
Example of reasonable follow-up protocol
Treatment of Type I Endoleaks
1. Type I endoleak is a high-pressure endoleak, thus warrants treatment whenever possible.
2. Management based on underlying mechanism :
– Migration : Leak may be sealed by insertion of an extension cuff
a) Proximal migration : Most aneurysms associated with migration have short necks, it may be challenging to place the extension cuff high enough to seal the leak and also maintain patency of the renal arteries
b) Distal migration : If progressive dilation of the distal landing zone makes it impossible to achieve a tight seal in the common iliac artery, it may be necessary to extend the stent-graft into the external iliac artery, which usually has a smaller diameter. If this is the case, to avoid a type II EL due to retrograde flow, the internal iliac artery should be occluded near its origin before insertion of the stent-graft extension.
– Neck dilation : Reinforcement of the proximal section of the stent-graft with a large Palmaz stent.
3. If endoluminal procedures are unsuccessful, late surgical conversion must be considered. Type I ELs are the most common causes of late surgical conversion after EVAR.
Treatment of Type II Endoleaks
1. Treatment plan depends on sac diameter :
– Persistent but a stable sac diameter : Conservative treatment
– Maximum sac diameter increases by >= 5 mm within a 6-month observation period : Requires treatment
2. For effective treatment, embolization of underlying inflow/outflow by three methods : – Transarterial arterial approach : Embolization should be performed directly in the sac at the center of the EL to occlude all in- and outflow vessels
( If only inflow artery is occluded, the outflow can be recruited as feeding artery )
– Percutaneous sac puncture : Through translumbar or transabdominal approach under USG guidance, embolization is then performed with coils, thrombin, and/or liquid embolization material
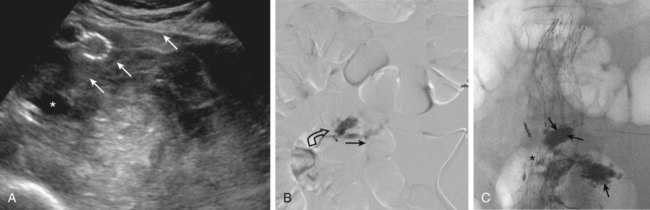
Example :
Transarterial treatment of a type II endoleak
– A : Type II EL ( * ) mainly fed by arc of Riolan and retrogradely perfused IMA ( open arrow ). Microcatheter has already been introduced into Riolan arc (arrow).
– B : Tip of microcatheter in center of EL and embolization is ideally begin from this position.
– C and D, Embolization has been performed with bucrylate, which was injected into sac, obliterating EL (open arrows). Thereafter, coil embolization of main trunk of IMA has been performed (solid arrow). Flow in EL was abolished.
Example :
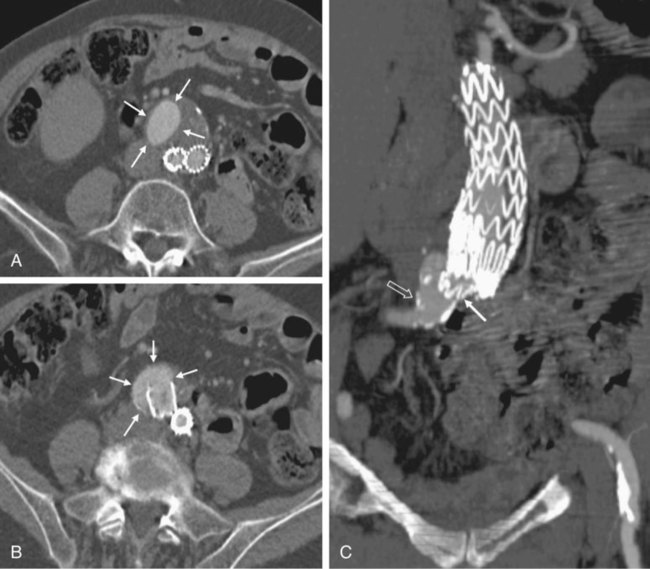
Treatment of a type II endoleak (EL) by direct sac puncture.
– A : Transabdominal puncture of a type II EL under sonographic guidance. Needle can be seen clearly under US (arrows). Tip of needle was guided into center of area of maximum perfusion ( * ).
– B : Direct contrast injection nicely displays EL. Inflow (open arrow) and outflow (solid arrow) vessels can be clearly seen.
– C : Bucrylate was injected directly into EL via transabdominal approach. Distribution of glue nicely reflects angioanatomic outline of EL (arrows).
Treatment of Type III endoleaks
1. Type III ELs are high-pressure ELs and require treatment when diagnosed
2. Typically, stent-graft separation is the cause, although rarely a graft tear can be the reason for the leak. Most type III ELs are treated by insertion of another stent-graft that lines the area of separation or graft tear.
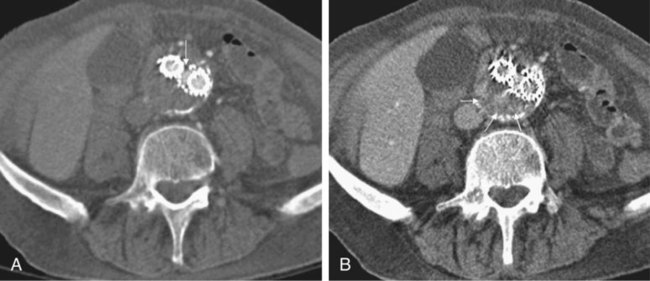
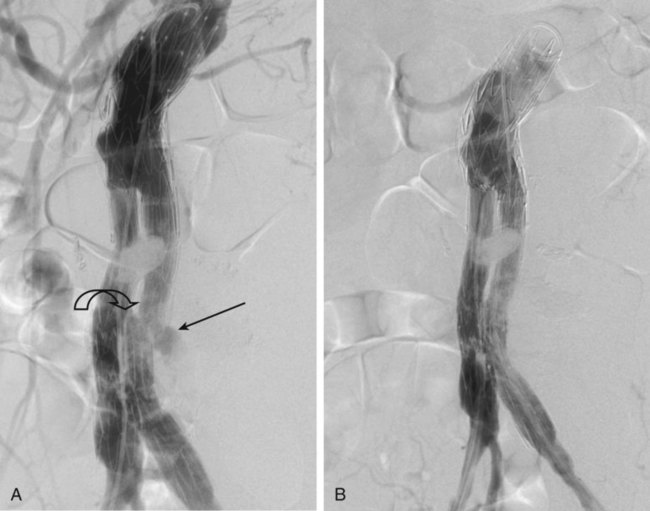
Example :
A : Double type III endoleak (EL) in a patient with detachment of both iliac limbs from main body of prosthesis (arrows).
B : Treatment with coaxial insertion of two stent-grafts in each limb.
Treatment of type V endoleaks
1. By definition, no specific leak can be detected, treatment is always non-focused and has no guarantee of success.
2. Treatment options include stent-graft relining with a coaxial system, most often with a monoiliac device. A surgical solution should always be considered if fails.

